TULSA-PRO Treatment for BPH
Organ and Function-Preserving Procedure
- TULSA-PRO Treatment for BPH
- TULSA-PRO Resection of the Prostate
- Patient Advantages with TULSA-PRO
- Preserving Natural Ejaculation
- Healthy Prostate
- Enlarged Prostate
- The TULSA-PRO Technique
- Advantages of the TULSA-PRO Technique
- Enlarged prostate before TULSA-PRO Prostate after TULSA-PRO
- MRI as a Prerequisite for TULSA-PRO
- Symptoms Associated with BPH
- Preliminary Diagnostic Procedures
- Treatment at the ALTA Klinik Using Outside MRI Scans
TULSA-PRO Resection of the Prostate
The world’s first minimally invasive TULSA-PRO resection of the prostate was carried out at the ALTA Klinik in March 2017. Since then, the ALTA Klinik has treated about 300 patients with TULSA-PRO.
Our aim in performing this procedure is to eliminate the symptoms associated with benign prostatic hyperplasia (BPH) in a minimally invasive manner so as to preserve the proper functioning of the prostate gland. This aim includes, in particular, preserving the capacity for natural ejaculation of the men who undergo the procedure while also avoiding erectile dysfunction and urinary incontinence.
Terminology:
TULSA stands for Transurethral ULtraSound Ablation.
The term transurethral means “through the urethra”. Ablation means the “removal of bodily tissue” – in this case via the targeted delivery of ultrasonic thermal energy. MRI stands for magnetic resonance imaging, a superior medical imaging technique that uses strong magnetic fields to produce three dimensional detailed images of anatomical structures without the use of ionizing radiation.
Benign prostatic hyperplasia (BPH) is an increase in the size of the prostate as a result of the proliferation of variously sized noncancerous nodules in the transition zone of the prostate. While the transition zone of the prostate in young men is scarcely discernible, it grows continuously as men age and can lead to annoying symptoms as it begins to compress other structures.
The costs for the TULSA-PRO therapy including the preliminary examinations are around 20.000 EUR (tax-free services).
Patient Advantages with TULSA-PRO
The TULSA-PRO procedure to resection the prostate offers patients a number of advantages:
- The procedure offers patients a means of retaining their capacity for natural ejaculation. This is because the ejaculatory ducts are left intact.
- The procedure offers patients a means of avoiding erectile dysfunction. This is because the neurovascular bundles in the prostate are left intact.
- The procedure offers patients a means of avoiding urinary incontinence. This is because the internal and external urethral sphincters are left intact.
- Prostate function can be preserved because the range of the treatment can be limited to the transition zone, i.e. prevented from damaging sensitive structures in the peripheral zone.
- The cooling system in the ultrasound applicator protects the urethra against thermal injury.
- The procedure permits the treatment of especially large volumes of prostate tissue.
Preserving Natural Ejaculation
Most of the transurethral procedures used to resection the prostate cause some degree of damage to the urethra and the ejaculatory ducts. As a result, the men who undergo the procedures are often left to face side effects that significantly compromise quality of life, including erectile and ejaculatory dysfunction (e.g. retrograde ejaculation, anejaculation).
In contrast, men who undergo the TULSA-PRO procedure are likely to retain a capacity for natural ejaculation because the scope of the tissue ablation does not include the ejaculatory ducts. Moreover, the cooling system in the ultrasound applicator protects the urethra against thermal injury.
Healthy Prostate
Enlarged Prostate
The TULSA-PRO Technique
The TULSA-PRO technique involves the insertion of an ultrasound applicator through the urethra and into the prostate gland to treat benign prostatic hyperplasia (BPH) via the targeted application of ultrasonic thermal energy.
The ultrasound applicator is outfitted with a linear array of 10 transducers that emit high-intensity ultrasound beams. Each transducer can be individually activated to enable the optimally circumscribed thermal resection of the prostate. For instance, the operator may choose to activate transducers 2 to 10 because their range corresponds to the dimensions of the excessive tissue growth in the prostate while leaving transducer 1 idle.
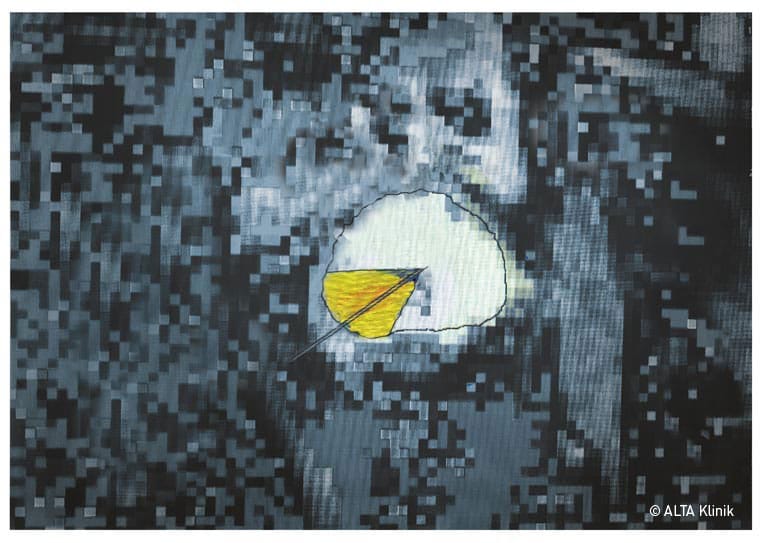
The TULSA-PRO procedure is MRI-guided and takes place in an MRI scanner. The preoperative planning for the procedure includes the use of up-to-date MRI scans to precisely demarcate the extent of the hyperplasia. This extent can then be entered into the system to control the exact range of the emitted thermal energy.
The ultrasonic energy emitted by the activated transducers ablates the excessive tissue in the transition zone of the prostate. The entire procedure is monitored and controlled in real time on a computer monitor.
Real-time monitoring of thermal development
The ablation treatment in the MRI scanner does not begin until the treatment zone has been precisely ascertained and the applicator has reached the optimal position. Once the transducers are activated, the applicator is rotated to bring about a uniform thermal ablation of the excess tissue in the transition zone of the prostate.
While the thermal energy emitted by the transducers on the applicator ablates the excess tissue in the transition zone of the prostate, the applicator’s integrated cooling system protects the wall of the urethra against thermal injury. As a precaution, an additional endorectal cooling device is deployed protect the rectal wall.
Advantages of the TULSA-PRO Technique
The illustration below is provided to help explain the advantages of the TULSA-PRO technique.
- The minimally invasive TULSA-PRO procedure enables the targeted resection of the enlarged transition zone of the prostate via the application of ultrasonic thermal energy while at the same time preserving normal organ function. This requires the use of up-to-date MRI scans to precisely demarcate the treatment area in the context of preoperative 3D planning.
- In order to preserve the patient’s natural capacity for ejaculation, we leave the part of the transition zone that includes the ejaculatory ducts untreated.
The TULSA-PRO procedure involves the insertion of an ultrasound applicator through the urethra into the prostate gland. This introduces the advantage of direct targeted treatment within the prostate, which effectively reduces the risk of damage to important surrounding anatomy such as the rectum and the urethral sphincters. - The ultrasound applicator is outfitted with a cooling system to provide continuous protection against thermal injury to the wall of the urethra.
As a precaution, the TULSA-PRO procedure also includes the use of an endorectal cooling device. This device helps to ensure the protection of neurovascular bundles against the long-term effects of the application of thermal energy. - The TULSA-PRO system enables high-precision planning and intervention, thereby ensuring that the distribution of thermal energy during the resection of the prostate extends only as far as the so-called surgical capsule (demarcation between the transition and peripheral zones of the prostate). The peripheral zone therefore remains protected against the application of thermal energy. This sort of control is possible with TULSA because the temperature in the designated treatment zone can be tracked in real time via MR thermometry on a computer monitor and adjusted accordingly throughout the procedure.
- TULSA-PRO enables a uniform ablation of the excess tissue in the designated treatment area inside the prostate.
With time the tissue that is coagulated during the procedure is removed from the body via the circulatory system. The symptoms associated with BPH subside.
Patient PSA levels also tend to drop back down into the normal range after the TULSA-PRO procedure.
The resection of the prostate is often followed by a general improvement in prostate function. This can be explained by the fact that the peripheral zone of the prostate, which was compressed before the procedure, is allowed to recover.
Enlarged prostate before TULSA-PRO Prostate after TULSA-PRO
MRI as a Prerequisite for TULSA-PRO
Multiparametric MRI of the prostate establishes a basis for a targeted TULSA-PRO resection of the prostate.
The necessary information provided by the MRI scan includes the following:
- Total prostate volume
- Extent of the BPH
- Disposition of the enlarged transition zone in relation to the urethra and the urinary bladder
- Disposition of the enlarged transition zone in relation to the peripheral zone
- Disposition of the neurovascular bundles and other sensitive structures
- Reliable basis for assuming the absence of prostate cancer, particularly in the peripheral zone
Symptoms Associated with BPH
The prostate gland undergoes changes as men age. Nearly every adult male approaching the age of 50 exhibits some degree of age-related benign prostatic hyperplasia (BPH), or prostate enlargement. The degree of the enlargement naturally differs from man to man. Moreover, while the enlargement may cause no more than moderate symptoms in some men, others are faced by a significantly diminished quality of life.
The enlargement arises from the proliferation of noncancerous nodules in the transition zone of the prostate, with the presence of symptoms generally depending on the extent of the enlargement. Given that the urethra passes through the transition zone, it is quite susceptible to compression as the excessive growth in the transition zone progresses. The following urinary problems can arise as the excessive growth presses on the urethra:
- More frequent urge to urinate with smaller volumes of urine
- Nocturia (the need to get out of bed at night to urinate)
- Excessive urge to urinate
- Urinary incontinence
- Post-void dribbling
- Burning sensation when urinating
- Weak urinary stream
- Difficult and lengthy urination
- Delayed urinary stream
- Interrupted urinary stream
- Urinary retention
In most cases, the symptoms worsen with time. BPH can also lead to other complications such as urinary bladder stones and obstructive nephropathy.
Preliminary Diagnostic Procedures
1. MRI scan:
Multiparametric MRI of the prostate is the basis for minimally invasive, organ and function-preserving TULSA-PRO resection of the prostate. This examination enables your doctor to gather all of the information that is necessary for a targeted resection of the prostate.
Based on the experience we have gathered over the course of many years, we carry out a special, optimized multiparametric MRI scan of the prostate.
2. Treatment:
The organ and function-preserving TULSA-PRO resection of the prostate can be carried out on the basis of the MRI scan.
Treatment at the ALTA Klinik Using Outside MRI Scans
The TULSA-PRO treatment can also be carried out using the results of an outside MRI scan of the prostate so long as the images meet the criteria for planning the minimally invasive, organ and function-sparing TULSA-PRO procedure. In order to make this determination, we will need to see a CD copy of the imaging material along with the radiology report.
 English
English
 Deutsch
Deutsch  Nederlands
Nederlands