Multiparametric MRI of the Prostate
Specialist for MRI Prostate Diagnostics Since 2009
- Multiparametric MRI of the Prostate
- MRI Scan of the Prostate and Entire Pelvic Region
- Prostate MRI at the ALTA Klinik
- MRI Scan Showing Prostate Cancer
- MRI Scan Showing Benign Prostatic Hyperplasia
- MRI Scan Showing Benign Prostatic Hyperplasia and Prostate Cancer
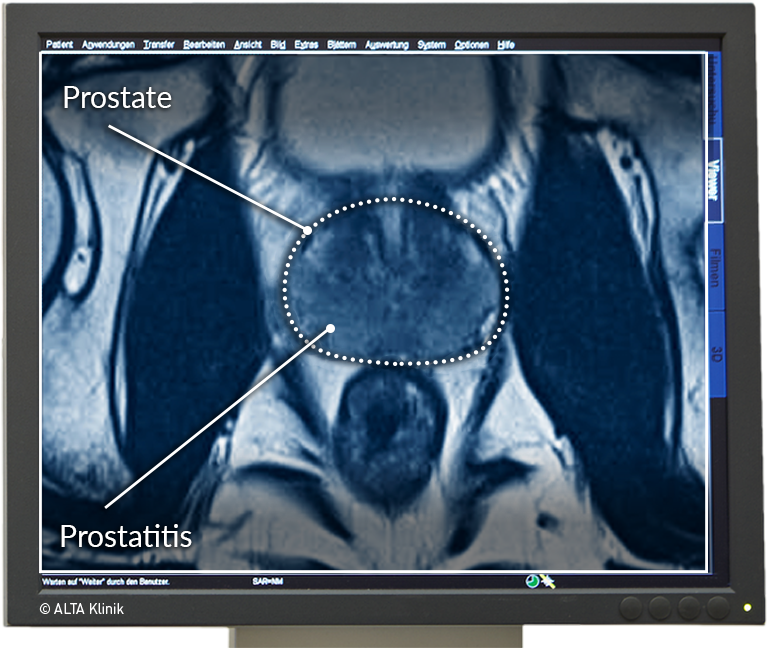
- MRI Scan Showing Prostatitis
- Early Detection Thanks to Prostate MRI
- Non-rectal, targeted 3-D live MRI-Biopsy of the Prostate – the optimized further development to the classical biopsy
- MRI/Ultrasound Fusion Biopsy
- Prostate MRI after Negative Needle Biopsy
- Prostate MRI after Ultrasound and a Digital-Rectal Exam
- Prostate MRI for Patients with a Family History
- MRI Prostate Status Check
MRI Scan of the Prostate and Entire Pelvic Region
What is the rationale for a multiparametric MRI scan of the prostate?
MRI scans of the prostate are carried out to determine the exact nature of any changes that have taken place in the prostate. Patients are usually made aware of such changes when PSA testing indicates that their PSA level is elevated (> 4ng/mL). Please refer to PSA Table to find out more about PSA levels.
An MRI scan of the prostate is in fact an ideal means of diagnosing changes in the prostate. This is because the images it generates enable your doctor to distinguish between the various benign, inflammatory and malignant diseases of the prostate, including benign prostatic hyperplasia (prostate enlargement), prostatitis and prostate cancer.
Prostate MRI is an especially advisable procedure if your PSA level has risen continuously over time or has spiked within a short period of time (e.g. within 6 months).
While your PSA level is an excellent indicator of change in your prostate, it alone does not provide a reliable basis for a diagnosis. This is because PSA levels tend to rise in response to a variety of different changes in the prostate. Moreover, while very high PSA levels are not necessarily worse than moderately high levels, they do increase the urgency of further diagnostic procedures.
Prostate MRI at the ALTA Klinik
Before performing the MRI scan, your doctor will meet with you to get to know you and to ask you questions about your medical history and any current symptoms you may have (e.g. a more frequent urge to urinate). As the patient, you will naturally be given ample opportunity to ask any questions you may have.
Multiparametric MRI scanners use magnetic fields, radio waves, field gradients and a computer to produce detailed images of the inside of your body. MRI does not involve the use of ionizing radiation (e.g. x-rays).
A computer processes the signals and generates a comprehensive series of high-resolution, cross-sectional images of the prostate. These images can be studied by your doctor from different angles so as to detect any abnormal or diseased tissue.
Thanks to the many years of experience we have gathered as specialists in the area of prostate diagnostics since 2009, we have been able to optimize our MRI-based examinations of the prostate. Such optimizations include the use of special examination techniques and additional measurements that are enabled with an MRI device of the latest generation. We use a fully equipped 3-Tesla MRI system known as the Siemens MAGNETOM Skyra.
Following the examination, our radiologists evaluate the images according to the Pi-Rads classification and show the MRI images to our patients, explaining our findings to them calmly and in simple terms. Depending on the specific results of the MRI examination, we also provide a comprehensive recommendation concerning the various treatment alternatives.
Our multiparametric MRI enables us to give our patients a maximum degree of diagnostic assurance.
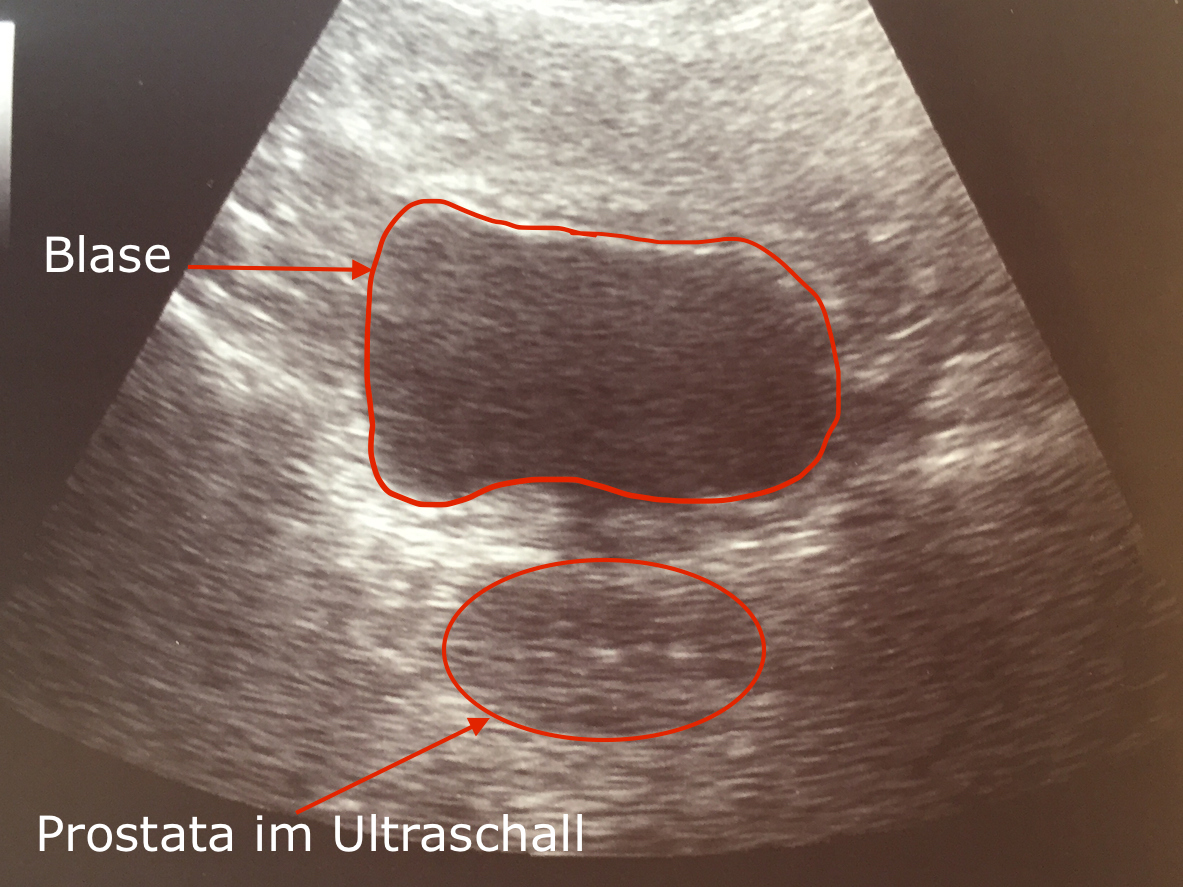
- Prostate with Ultrasound
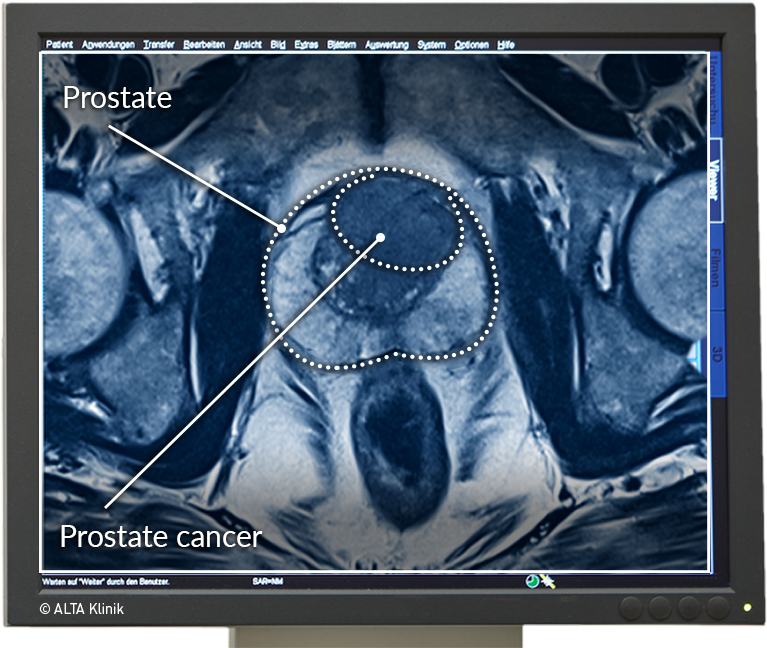
MRI Scan Showing Prostate Cancer
The image on the right shows a tumor that is relatively well-delineated from the surrounding healthy tissue.
Many men mistakenly assume that their risk of prostate cancer is higher if they are affected by benign prostatic hyperplasia. The reason for this mistaken assumption probably relates to the fact that both prostate cancer and BPH are diseases that occur in men far more frequently after they have reached their 40s. As it turns out, prostate cancer occurs just as frequently in men who exhibit only minimal BPH.
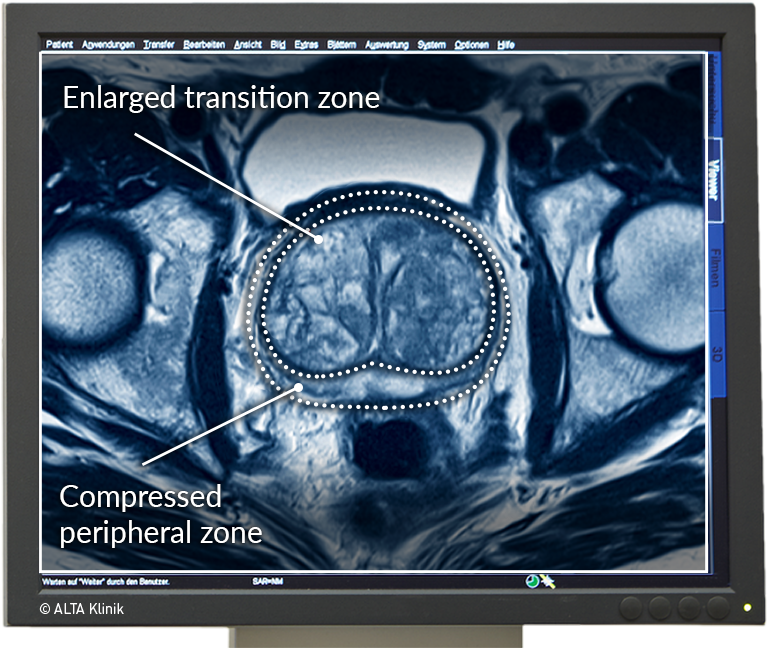
MRI Scan Showing Benign Prostatic Hyperplasia
While prostate enlargement, or benign prostatic hyperplasia, affects nearly all men by the time they reach their 40s, the enlargement does not automatically lead to an elevated PSA level. As it turns out, it often depends on the extent of the enlargement.
Benign prostatic hyperplasia (BPH) is an age-related change in the prostate that develops when benign nodules propagate in the transition zone of the prostrate, increasing the volume of the transition zone and pushing outward and effectively narrowing the peripheral zone.
Men with benign prostatic hyperplasia are typically affected by a more frequent urge to urinate and a weak urinary stream. This is because, in addition to pushing outward against the peripheral zone, the propagation of nodules in the transition zone can compress the urethra, which passes through the center of the prostate, and cause urinary retention.
MRI Scan Showing Benign Prostatic Hyperplasia and Prostate Cancer
It is important to also examine patients with known cases of BPH and steadily or abruptly rising PSA levels for the presence of prostate cancer. In contrast to BPH, early-stage prostate cancer is asymptomatic. In other words, it involves a malignant change in prostate tissue that men are not capable of noticing. In such cases, an elevated or rising PSA level is often the first warning sign.
There are also rare cases in which prostate enlargement is not caused by age-related BPH, but by a large, advanced-stage tumor.
MRI Scan Showing Prostatitis
Prostatitis typically affects the entire prostate gland and is usually immediately detectable in MRI scans. The classic symptoms of prostatitis include a burning sensation when urinating and a more frequent urge to urinate.
Early Detection Thanks to Prostate MRI
Prostate cancer is a disease that affects men as they age, with the likelihood of occurrence beginning to increase significantly at the age of 50. While prostate cancer typically leads to increased PSA levels, there are also cases in which patients show no more than slightly elevated PSA levels despite having a highly aggressive form of prostate cancer (e.g. with a Gleason score of 9). An MRI scan of the prostate can be extremely helpful in such cases because it will usually enable radiologists to precisely detect the tumor in question.
Non-rectal, targeted 3-D live MRI-Biopsy of the Prostate – the optimized further development to the classical biopsy
At ALTA Klinik we have developed the non-rectal, targeted 3-D live MRI-Biopsy of the Prostate. We developed the biopsy because we saw the cancer lesion in the MRI image and the patient got a negative biopsy result because the urologist was using the ultrasound as the imaging device. The ultrasound only showed the prostate from the outside and no prostate cancer areas. Thus, suspicious lesions cannot be hit and the patient was lulled into a false sense of security due to a negative biopsy (biopsy with no findings).
This is a problem that Lumiani, MD, and his team at ALTA Clinic have addressed by inventing their own targeted biopsy that is safer for the patient.

Patient during the non-rectal, transgluteal 3-D live MRI-Biopsy of the Prostate
Both the preliminary examination and the biopsy both take place in the MRI machine. By accessing via the gluteal muscle, all areas in the prostate can be hit. This procedure is painless for the patient, without preventive antiobiotic use and without general or partial anesthesia. Therefore, the patient can go home or to the hotel after the biopsy and does not need an inpatient stay in Bielefeld.
MRI/Ultrasound Fusion Biopsy
MRI/ultrasound fusion biopsy is an optimized form of conventional needle biopsy. Conventional needle biopsy involves the removal of 10 to 12 samples of prostate tissue using a standard template. Successful detection of an existing tumor using conventional needle biopsy is essentially a matter of chance.
In order to add a measure of precision to the sample-taking procedure, MRI/ultrasound fusion biopsy makes use of a special ultrasound device to merge previously captured MRI images with live ultrasound images. This enables your physician to use the MRI images for purposes of orientation, thereby increasing the likelihood of removing a tissue sample at a so-called area of interest.
Prostate MRI after Negative Needle Biopsy
If the result of a template-based biopsy is negative – meaning that no prostate cancer has been detected – the question naturally arises as to whether the conventional biopsy procedure simply failed to “hit” an existing cancerous lesion in the prostate.
The fact that this question arises demonstrates that it would have been smarter to first perform an MRI scan of the prostate, i.e. to determine the presence of areas of interest, before carrying out a biopsy.
Prostate MRI after Ultrasound and a Digital-Rectal Exam
It is generally difficult to detect tissue changes in the prostate using ultrasound. Moreover, digital rectal examinations permit assessments only of the region of the prostate that is closest to the rectum. If a patient exhibits an elevated or rising PSA level and the results of both the ultrasound and digital-rectal examinations are unremarkable, the only way to achieve an appropriate level of diagnostic reliability is to perform an MRI scan.
Prostate MRI for Patients with a Family History
The occurrence of prostate cancer is greater in men with a family history of the disease, especially if the family members in question are fathers or brothers. For those with a family history of prostate cancer, we recommend annual cancer screening in the form of PSA testing, as well as regular MRI examinations. If PSA testing reveals an increase in a patient’s PSA level, then an MRI scan can be arranged to determine the cause and thereby enable an early response to any conspicuous findings.
MRI Prostate Status Check
Many men are interested are in taking a preventive approach to maintaining good health. Given that prostate cancer is the most commonly diagnosed non-skin cancer in men, preventive care includes both prostate cancer screening in the form of PSA testing and a more extensive prostate status check. The prostate status check at the ALTA Klinik includes multiparametric MRI and comprehensive blood testing of all of the important parameters, including PSA, that are relevant to prostate health.
 English
English
 Deutsch
Deutsch  Nederlands
Nederlands